
The Eyes Have It
by Linda Aronson DVM
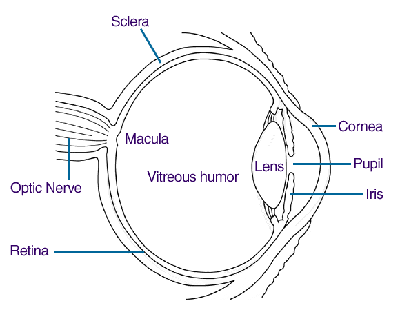
We are lucky in our breed that there are relatively few of the eye problems which plague collies and border collies among other breeds. Normally if we clean the accumulated crud from the corners of our beardies’ eyes each morning that pretty much covers eye care. Occasionally we will notice a little pus amongst the crud and have to deal with the infection. However, inherited eye problems do exist in beardies, and lest we become complacent we need only look at the closely related herding breeds and say there but for fortune… We are lucky in that we don’t have to rely on Dame Fortune either. The eyes of all dogs used for breeding, and preferably those of their closely related kin, should be checked by a board certified ophthalmologist every two years at least. Only by careful screening can we keep our breed’s eyes seeing clearly. It is sad that only 105 beardies underwent CERF examination in 2000. In this article I will look at the inherited eye problems that have been reported in beardies as well as some other non-inherited problems we may encounter. For only the second time in the history of this column we have a diagram.
Inherited Diseases
Juvenile Cataracts
The lens of the eye is a soft, transparent structure that shortens or lengthens to focus light beams on the retina at the back of the eye in order for the eye’s owner to see objects sharply whether they are close or far away. The capsule, a sort of sac, surrounds the lens, and supplies both shape and nutrition to the lens, which is without blood vessels. Cataracts are a cloudiness or opacity of the lens or capsule. Often people describe cloudiness in the eyes of old dogs as cataracts, but this is rarely the case. New fibers form at the periphery of the lens throughout life, to compensate the fibers towards the centre become increasingly dense and compact, this is called nuclear or lenticular sclerosis, this is not a cataract and does not cause blindness. It does give the eye a grey or silver cast. Cataracts can affect the whole eye or be localized. In beardies they are usually found on the anterior surface of the lens (closest to the front of the eye) at the top or bottom where the muscles attach to the capsule to change the lens’ shape, and they are under the capsule. However, other locations have been reported. While cataracts with genetic causes are programmed at birth, most cases of juvenile cataracts in beardies are picked up when the dog is between 2 and 5 years of age. The effect of these cataracts on the Beardie’s vision is usually mild, but bad enough that CERF recommends that affected dogs not be bred. At this point too little is known about the genetics of cataracts in beardies to speculate on the mode of inheritance. In other breeds for which there is more data, cataracts may be recessive, dominant or dominant with incomplete penetrance. In some breeds cataracts can progressively increase in size until the animal is blind, this has not been reported in beardies, although the degree of visual impairment is variable. Cataracts can occur that are not of genetic origin, most common causes are diabetes mellitus; infant/neonate milk replacement diets; uveitis and altered aqueous humor composition; retinal degeneration; persistent pupillary membranes; persistent hyaloid artery through the vitreous; electric shock; radiation; and various toxins. Some cataracts cause the eye to become inflamed and there will be excessive tearing and redness of the sclera (white of the eye). The dog may seem to squint especially in bright light. If left untreated this could progress to glaucoma or retinal detachment.
If the eye becomes seriously inflamed or the dog is blind, surgery called phacoemulsification sends ultrasonic shock waves through the eye to smash the lens. Sometimes a plastic lens is placed in the eye, but this only really improves near vision and is rarely helpful. Surgery results in 90-95% restoration of functional vision.
Progressive Retinal Atrophy (PRA)
The retina at the back of the eye is composed of receptor cells called rods and cones that respond by emitting nervous impulses when stimulated by light of different wavelengths. Rods respond in dim light, whereas the various types of cone respond to red, blue and green light. Not one but at least 6 distinct inherited forms of PRA have been described in many breeds of dogs and some mixed breeds. Ultimately PRA results in blindness. This is not a common disease in beardies and I am not sure that the type of PRA seen has been determined. In other breeds there is a test now for the gene mutation in Irish setters that causes rod cone dysplasia 1 (rcd1), as well as for a genetic marker for progressive rod cone degeneration (prcd). Prcd is the most widespread form of PRA and is found in poodles, cockers (American and English), labs, porties, Australian cattle dogs as well as many other breeds. Dogs with prcd form normal retinas, but they start to degenerate when the dog is about a year old, the dog first becomes night blind and then totally blind usually between 3 and 5 years of age. Because many dogs will have been bred before the disease can be detected the DNA test is particularly important, and can be used to detect both carriers and affecteds so that even the latter can be bred to clear mates so that puppies will be carriers but not affected by prcd. Because the test is for a gene marker rather than the mutation itself, the test may sometimes result in false positives. PRA in Irish setters (rcd1) and in Norwegian Elkhounds (rod dysplasia cone degeneration) is often apparent by the time the dogs are 6 weeks old, have diminished vision by 12 weeks and are completely blind by the time they are one or 2 years old.Because rods typically degenerate before cones the dog will be seen to stumble and bump into things in dimly lit areas before doing so in bright light. Their pupils tend to be dilated to catch as much light as possible. Dogs with PRA have fewer blood vessels on their retinas. This initial observation is followed up with an electroretinogram (ERG), which measures the amplitude of electrical signals given off by the retinal cells. This will be reduced in dogs with PRA.
In all breeds except the Siberian Husky, in which it seems to be a sex linked recessive trait, PRA is an autosomal recessive problem, i.e.. an affected gene must be inherited from both parents. Without a genetic marker it can remain hidden in the breed for a long time before suddenly cropping up.
Retinal Dysplasia
This is a retinal malformation that occurs when two of the embryological layers forming the retina fail to attach properly. In the mild form there will be folding of the inner layer of the retina, appropriately called "retinal folds". In the more severe form the layers do not attach at all, and there is complete or partial retinal detachment. Retinal dysplasia is not progressive, and can be detected in pups as young as 6 to 8 weeks old, although with puppies that small and wiggly getting a good view of the retina can be difficult. In most cases this is the result of a genetic defect, however, prenatal infection with herpes or parvovirus may also be causative. In many breeds simple autosomal recessive inheritance is suspected, in others a single, autosomal dominant gene causes both retinal dysplasia and skeletal changes. In many breeds, including beardies, there is insufficient data to speculate on mode of inheritance.Retinal folds produce small blind spots that rarely affect overall vision in dogs, but large areas or complete detachment result in major visual defects to complete blindness. In breeds like beardies where the condition is rare, and has not been found to produce major visual problems dogs with retinal folds may still be given CERF certificates, but if large areas of detachment exist the dog will not pass.
Retinal detachment is not necessarily hereditary. It can occur as a result of trauma (penetrating wounds or foreign bodies to the eye as well as blunt trauma), surgery to repair cataracts, or even spontaneously in dogs with mature cataracts or lens luxation. Various infectious agents (distemper, septicemia, bacteremia, leptospirosis, brucellosis, Rocky Mountain spotted fever, ehrlichia, Lyme disease, parasitic larval migration, toxoplasmosis, leishmaniasis, neospora and fungal and algal infections), immune mediated vasculitis, idiopathic thrombocytopenia, systemic lupus erythematosus and some toxic substances (griseofulvin - an antifungal agent, timethoprim-sulfa – an antibiotic, ethylene glycol – antifreeze poisoning) can all cause retinal detachment and subsequent blindness.
Persistent pupillary membranes (PPM)
These are a common finding in beardies, although at the last specialty the ophthalmologist conducting the CERF exams decided that some of those previously diagnosed in beardies were not PPM but actually "a normal branched blood vessel in the inner and outer surface of the iris {the colored part of the eye} which was closer to the surface than normal and mimicked PPM". Currently PPM does not prevent a Beardie from being given a CERF certificate. PPMs are remnants of the fetal pupillary membrane that covers the pupil before birth and provides a blood supply to the lens. In puppies at birth the pupillary membrane is still present and is gradually absorbed, normally disappearing by the time the puppy is four or five weeks old. If you look at the pupils of pups whose eyes have just opened you may see web like strands of the membrane.
When the strands don’t disappear they form PPMs. These may cross the pupil from iris to iris, run from the iris to the lens, or iris to cornea, or attach at one end to the iris with the other floating free. Strands can be single or forked. Iris to iris PPMs rarely cause a problem, and may continue to regress with age, but rarely disappear entirely. Those that attach to the lens’ capsule though can result in small cataracts, opacities on the lens, although these are non-progressive and rarely affect vision to any significant extent. Worse are those attaching to the cornea where they also produce opacity, but may also cause fluid to accumulate in the cornea (edema). If there are a lot of strands this can lead to blindness. As pups age the strands may regress and the blindness resolve, although the strands don’t disappear completely. Iris to iris PPMs are classified by CERF as a "breeder option" problem. Most are small and are probably sporadically occurring rather than hereditary defects. Breeding these dogs does not produce puppies with visual impairment. Breeding to unaffected dogs if possible may still be advisable. This is the current status of PPMs in beardies. However, there are breeds in which PPM is hereditary, and has been shown to produce blindness in offspring. Any PPM seen in these breeds will result in denial of a CERF certificate.
Distichiasis
Fortunately beardies aren’t affected by the more serious eyelid defects, entropion and ectropion, where the eyelid rolls in or out, respectively. Distichiasis describes the condition in which one or more eyelashes are directed in towards the eye rather than outwards. If it is only one or two eyelashes removing the offenders is sufficient. If there are more, surgery is needed to correct the defect, which can produce conjunctivitis, and more severe conjunctival abnormalities if left untreated. Usually in beardies only a few hairs are involved. If the hair under the eyes is often stained and you see an abundance of tearing, epiphora, you might suspect distichiasis or possibly a blocked tear duct. The latter may require surgical intervention.
Lipid corneal dystrophy
Is caused by the deposition of lipid in the body of the cornea. It is seen in young adult beardies, although the pattern of inheritance has not been determined. There is usually no inflammation or other symptom. Only in cases of extensive depositions will vision be impaired. Usually there will be a circular opacity in the center of the cornea that is grey, white or silver in color. It is probably the result of a localized error in corneal lipid metabolism, although elevated blood lipid levels can increase the size of the opacities, which usually occur symmetrically in both eyes. Usually no treatment is necessary. If the opacity interferes with vision then the lipid can be surgically removed.
Hypertrophy of the nictitans gland of the third eyelid has been reported as a hereditary problem in beardies. The third eyelid comes down over the eye to help protect it, and you can normally spot it in the corner of the eye. I have never come across this condition, but presumably it would result in the third eyelid permanently prolapsing totally or partially over the eye and would resemble the so-called "cherry eye", where the gland detaches from the periorbit of the eye.
Non-inherited eye conditions
I’m only going to cover a couple of the more common problems. Tumors of the eye itself (cancer of the orbit) are usually sarcomas or adenocanthomas and most are primary and malignant. By the time they are normally detected prognosis is poor. By contrast tumors of the eyelid are normally benign.
Red Eye
This is a general term used to describe a number of conditions that cause swelling and redness of the eyelids, redness of the conjunctival membranes (which line the eyelid and coat the white of the eyeball) or even hemorrhage within the eye. It can also have a number of causes; these include blepharitis (inflammation and swelling of the eyelids); conjunctivitis (inflammation of the conjunctival membranes); keratitis (inflammation of the cornea); inflammation of the sclera; anterior uveitis; glaucoma; disease of the eyeball; or hyphema (blood in front of the iris). The first three conditions are superficial and will involve superficial blood vessels in the conjunctiva that have a lot of branching, deeper layers have less branching. A discharge containing pus or pus and mucous also indicates a superficial problem, while a clear, watery discharge indicates a deep problem. Blepharitis can be congenital in some breeds in which eyelid abnormalities are inherited. In beardies causes would include trauma (especially cat claw marks); allergy (atopy, food, insect bites, inhalant, contact, drug, staph. hypersensitivity); autoimmune disease (pemphigus, lupus); bacterial infection (causes a sty like appearance); fungal, viral or parasitic infection; zinc or fatty acid deficiency; hypothyroidism, hyperadrenocorticism or diabetes; neoplastic or a variety of other problems! Clearly the first step is to find the cause rather than treat the symptom, but a good first step would be to flush the eye with saline solution, apply a warm washrag for 5-15 minutes 3 or 4 times a day, and clip the hair around the eye. Further treatment depends upon the cause, but most bacterial infections of the eyelid require systemic as well as topical antibiotics.Conjunctivitis is usually bacterial, but can also be viral, immune mediated or neoplastic, the result of trauma or foreign body irritation or secondary to dry eye or blockage of the tear ducts, a skin or other ocular disease. If there is a serious discharge the eye should be cleansed as for blepharitis and then the underlying cause addressed.Anterior uveitis is inflammation of the iris and/or the ciliary body, which attaches the iris to the choroid, the brownish layer between the sclera and retina. It is a common occurrence and has many causes including: diabetes, hyperlipidemia (excessive fat in the blood); elevated blood pressure; neoplasia (especially melanoma); cataracts; lens trauma or rupture; immune mediated vasculitis; immune mediated thrombocytopenia; algal, bacterial (including brucellosis, leptospirosis, Lyme disease or any systemic infection), viral, fungal or protozoal infection; trauma – especially blunt penetrating injuries; radiation; or blood clotting disorder. All cases of anterior uveitis should be rigorously investigated to discover the underlying cause. Topical +/-subconjunctival steroid or non-steroidal anti-inflammatory drugs are indicated in severe cases. Other treatment is cause dependent. Glaucoma is an increase in pressure within the eye as a result of reduced drainage of aqueous humor; this may be inherited and result from a narrowed drainage channel or secondary to another eye problem - lens luxation, anterior uveitis or hyphema. Inherited glaucoma has not been reported in beardies. It is a painful condition, the cornea is cloudy, the pupil dilated and there is a sudden loss of vision. As the disease progresses the eye will start to bulge. While treating the underlying cause is important, topically applied timolol reduces the production of aqueous humor; a diuretic may also be administered. Mannitol may be used to dehydrate the vitreous humor. In dogs in which anterior uveitis is not the inciting factor pilocarpine is applied to constrict the pupil and improve flow of aqueous humor.
Hyphema - blood in the aqueous humor - can result from trauma, retinal detachment, a tumor of the iris, ciliary body or choroid; uveitis especially from a rickettsial infection (ehrlichia, RMSF); blood clotting disorder; immune mediated vasculitis; systemic high blood pressure – either primary or secondary to kidney disease; or abnormal parasite migration. Treatment of the causative factor is indicated.
Corneal ulcers, degeneration and infiltration
These all cause opacity of the cornea. Ulcers are the result of erosion of the cornea secondary to inflammation. Ulcers can be superficial or deep and may be complicated by infection or the presence of degradative enzymes that can cause "melting" of the cornea and rapid spreading of the ulcer. In beardies trauma or foreign bodies in the eye are probably the most likely cause of ulcers, although dry eye, distichiasis, infection or paralysis of the eyelid - so that the cornea is not coated with tears and becomes dry and brittle - are all possible. Ulcers are diagnosed by applying fluorescein dye, which they retain. Topical antibiotics are usually applied as well as acetylcysteine to prevent "melting" ulcers. Therapeutic contact lenses may act as a kind of bandage to protect the healing cornea. Topical corticosteroids should not be applied. To repair deep ulcers surgical placement of a flap of conjunctival tissue may give the best chance of success. The cornea may be inflamed and yet not retain fluorescein. The cornea may become stained pinkish white and the eye is often painful causing tearing, squinting, blinking and rubbing at the eye. Nonulcerative inflammation of the cornea is probably immune mediated and treatment is directed at managing the signs rather than at producing a cure. Corneal degeneration or infiltration by lipid or calcium deposits is not inherited, and distinct from corneal lipid dystrophy. Lipid deposits are seen most often in dogs that are hypothyroid. There’s usually an associated inflammation, blood vessels and pigmentation also appear. The deposits are grey or white and may be circular, arced or irregular. The condition may progress to form ulcers and these should be treated accordingly, as should any underlying causative condition. A low fat diet may reduce lipid deposition. If the dog appears painful or its vision is impaired scraping the cornea or removing the outer layer of the cornea will help resolve the condition.
The eyes are the windows of the soul. I have barely scraped the surface in looking at potential problems, and yet as I said at the beginning our beardies are fortunately not plagued with major ophthalmic problems, and we should do everything we can to keep it that way. Which leads to the question that I’m sure everyone who’s stuck with me thus far is dying to ask. Should we tie back our beardies’ hair or let it flop over their eyes. Obviously the answer is … it depends. The original beardies had far less hair than our heavily coated dogs do now, their hair flopped down and protected their eyes from trauma as they ran through gorse and bushes, it kept out dust and mud and too bright sun. Now if our dogs are bumping into things all the time, or really need to see well, to avoid bumping the top rail of a jump, tying their hair back is an advantage. If my beardies are anything to go by, you can tie back most of the hair, but within a short while wisps will break away and flop down over the eyes providing enough cover to help shield the eyes from sticks and dust, but not enough to seriously impede their vision, and that is probably about the way it should be. I don’t like trimming the hair away as I think it does make the eyes more vulnerable, thinning is an option some people take, and if it’s not a show dog there’s no harm in that, in my opinion.
Copyright © 2002 [ Linda Aronson DVM].
All rights
reserved